Bariatric (Weight-loss) & Metabolic Surgery
- What is bariatric and metabolic surgery?
 Bariatric surgery is surgery that is performed with the intention of inducing weight loss. These operations have been found to have significant benefits for patients suffering from chronic metabolic conditions like diabetes mellitus, providing even remissions in certain instances, which seem to be independent of weight loss. In lieu of these benefits, bariatric surgery has acquired a re-defined name in metabolic surgery.
Bariatric surgery is surgery that is performed with the intention of inducing weight loss. These operations have been found to have significant benefits for patients suffering from chronic metabolic conditions like diabetes mellitus, providing even remissions in certain instances, which seem to be independent of weight loss. In lieu of these benefits, bariatric surgery has acquired a re-defined name in metabolic surgery.
These operations encompass a range of medical operations that are very different from cosmetic operations like liposuction and abdominoplasties (tummy tucks).
- How do bariatric operations work?
- Broadly speaking, there are 2 classifications of bariatric operations: restrictive and malabsorptive.
Restrictive operations work by reducing the storage capacity of the stomach, inducing early satiety (early fullness from a small portion of food) and eventual weight-loss through caloric restriction through portion control. These operations include the laparoscopic sleeve gastrectomy, laparoscopic Roux-en-Y gastric bypass and the laparoscopic adjustable gastric band.
Malabsorptive operations reduce caloric absorption through the reduction in the absorptive capacity of the intestines, normally through a series of “short-circuits”. Operations that employ malabsorption for induction of weight loss include the biliopancreatic diversion and the duodenal switch.
Restrictive operations are more commonly performed worldwide, as patients who have undergone these procedures have a better quality of life, without the potential malnutrition and debilitating diarrhoea that can complicate malabsorptive procedures.
- Am I eligible for bariatric surgery?
- Body mass index (BMI) is used as a criterion for those wishing to have bariatric surgery. BMI is calculated by dividing weight (kg) by height squared (metres squared, m²): BMI = kg/m². Criteria for bariatric surgery:
- BMI >35
- BMI >32 with obesity-related medical conditions
- What are my options for weight-loss?
- The management of obesity is tailored to the BMI of the individual. Medical and conservative (non-operative) measures are effective for those with a lower BMI, bearing the lowest risks of complications.
However, surgery is the only treatment that has been able to reliably allow the morbidly obese (BMI>32) to lose enough weight to treat medical problems. Dietary compliance, regular exercise and behavior modifications are still essential post-operative strategies to maintaining a healthy weight loss following surgery.
- What are the medical and conservative (non-operative) options in weight-loss?
- Non-surgical options for weight-loss include the following:
- Diet
- Exercise therapy
- Behaviour modification
- Medication
These modes of treatment are all important in maintaining a healthy weight, either as part of a surgical weight-loss programme, or on itself for the management of overweight.
- What bariatric surgical option is best for me?
- There are several effective operations for obesity. Our goal is to help you find the surgery that is best for you. We educate patients about the pros/cons and risks/benefits of each surgery and, in most cases, let our patients choose. However, for some patients, particularly those who are at a higher risk for surgical complications, one surgery may be recommended over the others.
At the Clinic, we usually perform restrictive operations where the capacity of the stomach is reduced, allowing the patient to be satisfied after a smaller portion of food and losing weight as a result. The three primary restrictive operations are the laparoscopic sleeve gastrectomy, laparoscopic Roux-en-Y gastric bypass and the laparoscopic adjustable gastric band.
It is essential to understand that there is no operation that will lead to weight loss without a sensible diet and exercise. Choosing an operation will depend on your needs, your medical conditions and your lifestyle.
- What are the pros/cons of the laparoscopic sleeve gastrectomy?
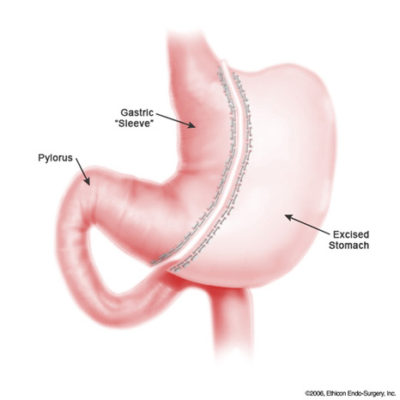 The sleeve gastrectomy is the procedure where a portion of the stomach along the outer edge is removed with surgical staplers, leaving a small remnant. The stomach is hence converted into a narrow tube, allowing smaller meal portions.
The sleeve gastrectomy is the procedure where a portion of the stomach along the outer edge is removed with surgical staplers, leaving a small remnant. The stomach is hence converted into a narrow tube, allowing smaller meal portions.
Weight loss occurs as a result of smaller meal portions, and the 5-year weight loss is estimated to be 60% of the excess weight (calculated as the current weight minus the ideal weight based on BMI). Patients who undergo the sleeve gastrectomy do not require as many nutritional supplements as those undergoing the bypass, but vitamins and minerals are still recommended after surgery. There is also no risk of device failure associated with the gastric band. While this operation is not reversible, it can be converted to a gastric bypass or duodenal switch if the patient requires even more weight loss.
There are, however, certain risks associated with the sleeve gastrectomy. These include an up to 1.5% risk of leakage and bleeding from the stapler line, which can potentially lead to a complicated repeat operation, and an associated 0.2% risk of mortality. Long-term risk of tube narrowing is very low, and this can normally be managed with non-invasive methods.
- What are the pros/cons of the laparoscopic Roux-en-Y gastric bypass?
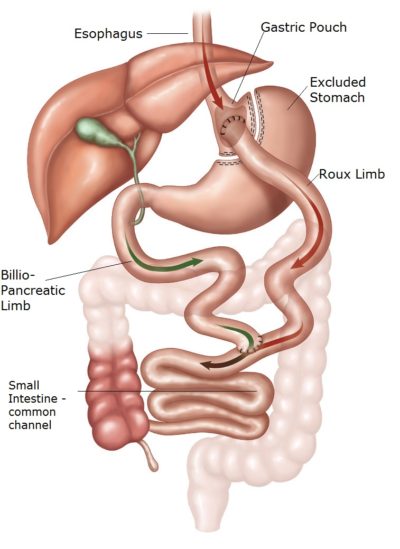 In the gastric bypass, the stomach is also reduced in size into a smaller stomach pouch that is, in turn, rewired to a segment of small intestine. The smaller stomach allows small meals to be taken. The rewiring makes it unpleasant to consume food of high sugar content, resulting in abdominal bloatedness and faintness.
In the gastric bypass, the stomach is also reduced in size into a smaller stomach pouch that is, in turn, rewired to a segment of small intestine. The smaller stomach allows small meals to be taken. The rewiring makes it unpleasant to consume food of high sugar content, resulting in abdominal bloatedness and faintness.
The result of this intestinal rearrangement has been found to be beneficial in helping patients with diabetes decrease their reliance on medication. 5-year excess weight loss ranges from 50 to 70%.
Being a more complicated procedure, the risks are slightly higher including leakage, bleeding and intestinal obstruction. There are also long term risks of malnutrition, intestinal obstruction and ulceration. As most of the stomach and part of the small intestine is bypassed, patients must take vitamins and supplements for the rest of their lives.
- What are the pros/cons of the laparoscopic adjustable gastric band?
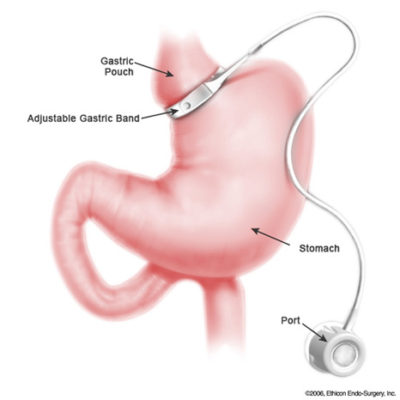 The gastric band is a procedure where a restrictive band is placed at the upper end of the stomach. This allows patients to feel satisfied after taking a small amount of food, even though the stomach remains the same size. The band can also be adjusted such that it takes longer for the food to reach the rest of the stomach, slowing down its transit and eating less than what others can do in the same amount of time.
The gastric band is a procedure where a restrictive band is placed at the upper end of the stomach. This allows patients to feel satisfied after taking a small amount of food, even though the stomach remains the same size. The band can also be adjusted such that it takes longer for the food to reach the rest of the stomach, slowing down its transit and eating less than what others can do in the same amount of time.
Gastric banding offers the lowest risk of mortality as a result of surgery, and this has been estimated to be about 1 in 1000–5000 patients.
However, it requires much effort to be effective, and has a significant rate of band erosion and slippage, both of which require repeat surgery. Such revision surgery has been estimated to be required in almost 17% of patients. 5-year excess weight loss ranges between 30–50% in most long-term studies.
- How are these bariatric operations performed?
- Bariatric operations are routinely done via laparoscopy (key-hole), where the access into the abdominal cavity is through small incisions on the abdominal wall. Laparoscopic surgery offers smaller scars, less pain and faster recovery compared to conventional open operations.
- What else is required before having a bariatric operation?
 Patients wishing to undergo bariatric surgery will be required to undergo endoscopy of the stomach (gastroscopy) to exclude any incidental stomach problems. There will be reviews by the anaesthetist and other specialists in the bariatric team, if necessary.
Patients wishing to undergo bariatric surgery will be required to undergo endoscopy of the stomach (gastroscopy) to exclude any incidental stomach problems. There will be reviews by the anaesthetist and other specialists in the bariatric team, if necessary.
Patients will also be required to undergo a very low caloric diet (VLCD) 2 weeks prior to the bariatric operation, which are liquid meal replacements. No other food is allowed, as this period is essential to decrease the size of the liver, which can potentially hamper the view during the operation.
- How long is the recovery time following bariatric operation?
- The average length of stay after surgery for the laparoscopic sleeve gastrectomy and laparoscopic Roux-en-Y gastric bypass is similar at 3–5 days after surgery. Patients who had a laparoscopic adjustable gastric band normally stay for 1 day after surgery.
Many patients who have sedentary jobs return to work within 2–4 weeks, but those with jobs requiring more physical effort may be out of work for 4–6 weeks.
- What should I expect after bariatric surgery?
- Bariatric operations are all performed under general anaesthesia, and only the heftiest patients require high dependency or ICU care. Fluids are generally started the day after surgery, and maintained until 2 weeks where soft diet is started. A regular diet is thence commenced at about 4 weeks after surgery.
- What are the potential benefits after bariatric surgery?
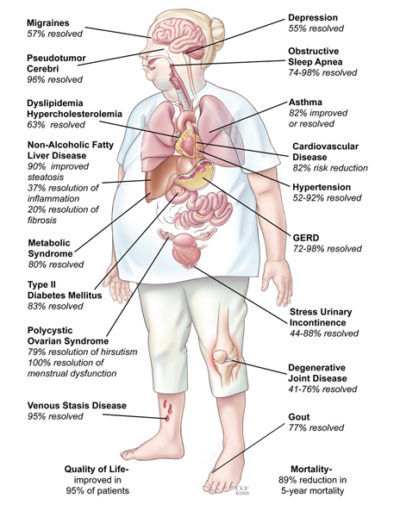 While there are obvious risks associated with bariatric surgery, the potential benefits outweigh these risks, as far as long-term studies have shown. Nevertheless, having any surgery is a major, life-changing decision that involves weighing the risks and benefits.
While there are obvious risks associated with bariatric surgery, the potential benefits outweigh these risks, as far as long-term studies have shown. Nevertheless, having any surgery is a major, life-changing decision that involves weighing the risks and benefits.
The following are well-documented health benefits achieved with bariatric surgery:
- Diabetes: 86% patients have an improvement in diabetic control, with 76% not requiring anymore medication
- Hypertension: 61% of patients have complete resolution of hypertension, while blood pressure control improves in 78%
- Hyperlipidaemia: lipid control improves in 70%
- Sleep apnoea: resolves in 85% of patients, and improved in 83%
- Quality of life: patients who lose weight feel lighter, and empowered to enjoy more physical activity, and less time attending medical consultations for their medical problems
- Life expectancy: long-term population studies have shown that obese individuals who undergo bariatric surgery have a longer life expectancy compared to those who have not done so