What is an ERCP?
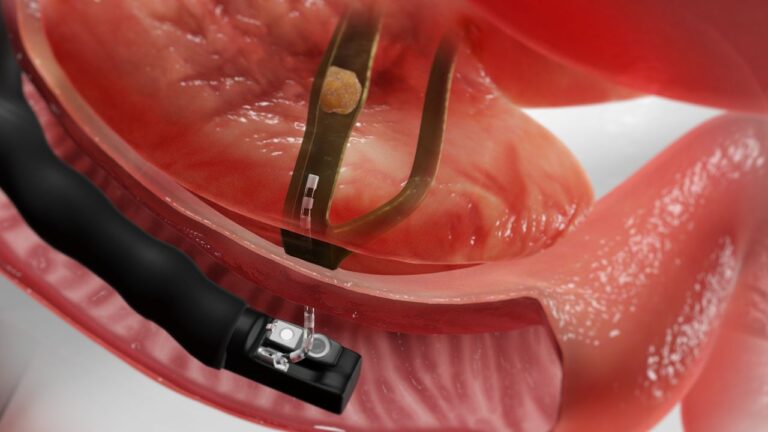
(ERCP) Endoscopic Retrograde Cholangio-Pancreatography is a procedure that utilises a bendable,
lighted endoscope with fluoroscopy (X-ray imaging) to examine and treat issues related to ducts that
drain the liver, gallbladder, and pancreas. The endoscope is inserted through the mouth and gently moved down the throat into the oesophagus, stomach, and duodenum (1st part of small intestine)
until it reaches the bile duct and pancreatic duct openings that drain into the duodenum.
Why is an ERCP performed?
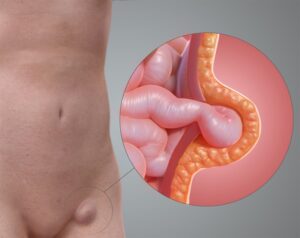
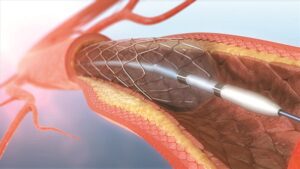
The most common indication for ERCP is to investigate and treat narrowing or blockage of the bile duct or pancreatic duct. This can be due to stones or growths at the bile and pancreatic ducts. Stones
can be removed using balloons or baskets. A tube (stent) may be placed in the duct to relieve the blockage during the procedure.
What preparation is required?
The stomach should be completely empty, and you should have nothing to eat or drink approximately
6 hours before your examination. Certain medications need to be adjusted or avoided before the
examination, so it is best to inform your surgeon of all your current medications as well as allergies. If
you also have any major diseases, such as heart or lung diseases, please also discuss this as you might
require special attention during the procedure. To reduce the risk of bleeding, you may be advised to
stop consuming any blood thinning medications prior to ERCP.
What can be expected during ERCP?
This procedure is usually carried out in a face-down position. You will have your throat sprayed with a
local anaesthetic before the test begins. Sedation or general anaesthesia is needed depending on your
medical conditions and complexity of the procedure. This is to ease discomfort, pain and anxiety. Your
heart rate, breathing and blood pressure will be closely watched throughout the procedure.
Depending on the reason for performing ERCP, your doctor may remove stones, take tissue samples or insert a stent into your bile / pancreatic duct. The procedure is expected to take about 1 hour.
What happens after ERCP?
You will be monitored closely in the ward for any complications after the procedure. You may
experience some throat discomfort or bloating. This is normal and should resolve quickly. If a stent
was inserted, you will be given advice on when to remove the stent. It is possible that the back of your throat will feel a little sore for a day or two afterwards.
What complications can occur?
ERCP is generally a safe procedure. The list of complications included is not meant to be exhaustive.
Any complications may possibly lead to prolonged hospital stay, long-term disability and even death. Possible complications include:
- Perforation 0.5% (tear) of the lining of the stomach or duodenum may occur and this can be treated with bowel rest, antibiotics and intravenous fluids. Surgery may be required to repair the perforation.
- Pancreatitis 5% (Inflammation of the pancreas) may occur due to irritation of the pancreatic duct during ERCP. This is often treated with bowel rest and pain relief medicines. Occasionally, pancreatitis can be severe enough to be fatal.
- Haemorrhage 2% (bleeding) may occur at the site where the bile and pancreatic duct opens into the duodenum. This happens most likely due to widening of the bile duct by small amounts of cutting (sphincterotomy) and/or stretching (sphincteroplasty) performed through the endoscope in order for treatment to be done. This sometimes resolves on its own without requiring treatment. If the bleeding is persistent, endoscopy treatment may be performed, for example using adrenaline injection, clip or blockage of the bleeding vessel (embolisation). Occasionally, blood transfusion may be required if significant bleeding occurs.
- Cholangitis 1% (infection of the bile duct) may occur due bacteria enter the bile duct following endoscopic manipulation. This can be treated with antibiotics and bile duct stent insertion.
- ERCP may sometimes be unsuccessful < 10% due to failure to pass the catheter through the bile or pancreatic duct. The procedure may need to be repeated in certain situations.
Are there any alternatives to the ERCP?
- Percutaneous transhepatic biliary drainage (PTBD)
Percutaneous transhepatic biliary drainage (PTBD) is insertion of a tube through the skin under the
ribs into the bile ducts. This is done usually under ultrasound guidance or other imaging tests. PTBD is
often done in patients who are not suitable for ERCP. This group of patients include those who have
surgically altered anatomy preventing the endoscope gaining access to the biliary tree and those in
whom ERCP was unsuccessful. PTBD permits a number of therapeutic interventions including drainage
of infected bile, extraction of biliary tract stones, dilatation of biliary strictures or narrowings, or
placement of stent across these strictures or narrowings. - Surgery
Surgery with intra-operative bile duct exploration is more invasive and has a longer recovery
compared to ERCP. This procedure is usually reserved for more complex situations eg multiple large
bile duct stones.