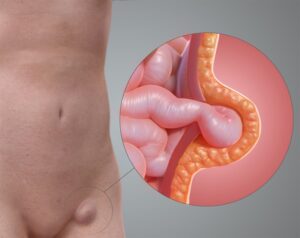
What are piles?
Piles (also called haemorrhoids) are swollen veins located in the lower rectum and anus, which
result from a variety of causes. They can be located either inside the rectum (internal
haemorrhoids) or just under the skin around the anus
(external haemorrhoids).
How do I know if I have piles?
The most common symptom is painless bleeding during bowel movement, which can range from a streak on the toilet paper to a splash in the pan.
Internal piles have delicate surfaces that bleed upon contact with the movement of stools, and especially so when stools are hard when one is constipated. When piles enlarge, straining on bowel
movement can cause them to protrude beyond the anal opening, giving rise to prolapsed piles.
Prolapsed piles can be a source of discomfort, pain (when strangulated of its
blood supply) or irritation / itch.
External piles can itch or bleed when irritated. Occasionally, they can form as a result of blood pooling under the skin, causing sudden pain and swelling
(perianal haematoma).
Other symptoms include:
- lumps around the anus
- anal pain or discomfort
- anal itch or irritation
- leaking of faeces
What causes piles?
Veins in the lower rectum and anus are a normal physiological feature, but these veins will swell in response to increased pressure in the lower rectum. The
causes for increased pressure include:
- straining during bowel movement
- prolonged sitting on a toilet
- chronic diarrhoea or constipation
- obesity
- pregnancy
- anal intercourse
When should I consult a doctor?
While rectal bleeding is the most common symptom of piles, not all rectal bleeding is caused by piles. Do not assume rectal bleeding is from piles until you get it checked out by a doctor. The symptoms of colon and rectal cancer are similar to those of piles, and only the appropriate investigations will be able to
distinguish these two very different conditions.
If the bleeding is excessive, or if you experience shortness of breath or light-headnessness from it, it might just mean that your blood reserves are low.
You will certainly be advised to seek urgent medical attention then.
If the bleeding is not a fresh red, but a dark maroon or black, or is accompanied with other
symptoms like difficulty passing motion or a change in bowel habits, you should also get it checked out by your doctor.
Your doctor will be able to do a thorough medical examination after finding out more about the
circumstances around the piles, before suggesting the
appropriate treatment.
What are the potential complications of piles?
In addition to excessive bleeding which can lead to anaemia and consequent weakness and faintness, piles that have prolapsed can also be complicated with
strangury.
Strangulation of piles occurs when the blood supply is cut off, often after it has prolapsed. Upon strangulation, it swells further and can lead to gangrene.
What should I expect from a consultation with the doctor?
The doctor will start with a detailed interview on your medical background before asking about the circumstances around the current problem of piles. A physical examination will then be performed, which includes a rectal examination. The rectal examination is not painful, and is required to visualise
the lower rectum and anal canal for the presence of internal piles.
Based on the history and physical examination, your doctor will then proceed to propose a
management plan, which may include a thorough examination of the colon with a colonoscopy. This might be required if you are at risk of having colorectal cancer, or if your symptoms are suggestive that you might have
another digestive problem.
What are my treatment options?
Depending on the severity, your doctor may propose one of three available options
- Medication and lifestyle changes
- Medication can help to smoothen bowel movement (lactulose, fybogel), as can dietary fibre by increasing the consumption of fruits, vegetables and unprocessed cereal
- Medication may also be given to normalise the venous circulation (Daflon; micronised purified flavonoid fraction), to alleviate the symptoms of bleeding and discomfort caused by piles
- Creams and suppositories can occasionally be given to alleviate mild itch and discomfort on a temporary basis
- Increasing dietary fibre to improve bowel movement should be taken, to decrease the need to strain. Prolonged toileting sessions should be avoided by discouraging unnecessary concomitant habits of reading while on the toilet seat
- Rubber band ligation
- Tiny rubber bands can be placed over the base of the swollen veins (piles), causing them to wither and fall off. Ligation is simple and effective, but is limited by the size of the piles. There is some mild discomfort and tenesmus (feeling of wanting to open bowels) for about 2-4 days after the procedure, before the ligated piles fall off. There can occasionally be some bleeding when the piles fall off, but this is normally mild and stops spontaneously.
- Surgery
- Surgery is required if the piles are complicated (prolapsed, strangulated or gangrenous) or too large to be ligated by the rubber bands