What is Gastroscopy?
Gastroscopy (also known as upper endoscopy, OGD or
oesophagogastroduodenoscopy) is a procedure that enables your surgeon to
examine the lining of the oesophagus (swallowing tube or food pipe), stomach and
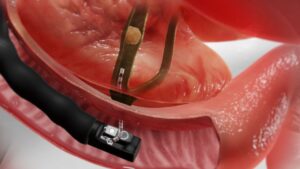
duodenum (first portion of the small intestine). A bendable, lighted tube about the
thickness of your little finger is placed through your mouth and into the stomach and
duodenum.
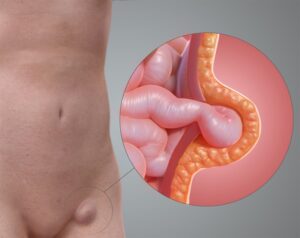
Why is a Gastroscopy Performed?
Gastroscopy is performed to evaluate symptoms of persistent upper abdominal pain or discomfort, nausea, vomiting, difficulty swallowing or heartburn. It is an excellent
method for finding the cause of bleeding from the upper gastrointestinal tract, and
also to evaluate the oesophagus or stomach before and after major surgery. Upper
endoscopy can detect early cancer and can distinguish between cancerous and
non-cancerous conditions by performing biopsies of suspicious areas. Biopsies are
taken by using a specialised instrument to sample tissue, which are then sent to the
laboratory to be analysed. A biopsy is taken for many reasons and does not mean
that cancer is suspected.
What Preparation is Required?
The stomach should be completely empty, and you should have nothing to eat or
drink approximately 6 hours before your examination.
Certain medications need to be adjusted or avoided before the examination, so it is
best to inform your surgeon of all your current medications as well as allergies. If
you also have any major diseases, such as heart or lung diseases, please also discuss this as you might require special attention during the procedure.
You will be sedated during the procedure, so please arrange to have someone drive
you home after. You should not drive or operate machinery until the next day.
What can be expected during the Gastroscopy?
You will have your throat sprayed with a local anaesthetic before the test begins and medication will be given through a vein to help you relax during the examination. You will be laid on your side as the endoscope is gently passed through your mouth to complete the examination. Air is introduced into your stomach during the
procedure to allow a better view of the stomach lining. The procedure usually lasts
15-30 minutes. The endoscope does not interfere with your breathing, and most
patients fall asleep during the procedure. A few find it only slightly uncomfortable.
What happens after Gastroscopy?
You will be monitored in the endoscopy suite for 1-2 hours, until the effects of the
sedatives have worn off. Your throat may be a little sore for a day or two, and you
may feel bloated immediately after the procedure because of the air that is
introduced into your stomach during the examination. You will be able to resume
your diet and take your routine medication after you leave the endoscopy area,
unless otherwise instructed. Your surgeon will inform you of the test results on the
day of the procedure, unless biopsy samples were taken. These results take several
days to return. If you do not remember what your surgeon told you about the
examination or follow-up instructions, call the Clinic to find out what you were
supposed to do.
What complications can occur?
Gastroscopy and biopsy are generally safe. While complications are rare, they can occur. They include bleeding from the site of a biopsy or polypectomy and a tear (perforation) through the lining of the stomach or intestinal wall. Blood transfusions are rarely required. A reaction to the sedatives can occur. Irritation to the vein that medications were given is uncommon, but may cause a painful lump lasting a few
weeks. Warm, moist towels will help relieve this discomfort.
It is important to recognise the early signs of possible complications and to contact
the Clinic if you notice symptoms of difficulty swallowing, worsening throat pain, chest pains, severe abdominal pain, fevers, chills or rectal bleeding.
Are there any alternatives to Gastroscopy?
A double contrast barium meal examination is an alternative, but it is not as
informative as a gastroscopy, and has the added disadvantage that tissue samples
cannot be taken, and the potential risks associated with x-ray exposure.
It involves swallowing barium (a white chalky liquid) which is then followed with the
x-ray scanner while it makes it transit down the upper gastrointestinal tract.