What is a colonoscopy?
Colonoscopy is a procedure that enables your surgeon to examine the lining of the
rectum and colon. A soft, bendable tube about the thickness of the index finger is gently inserted into the anus and advanced into the rectum and colon.
Why is a colonoscopy performed?
A colonoscopy is usually done 1) as part of a routine screening for cancer, 2) in
patients with known polyps or previous polyp removal, 3) before or after some
surgeries, 4) to evaluate a change in bowel habits or bleeding or 5) to evaluate
abdominal pain or discomfort.
What preparation is required?
The rectum and colon must be completely emptied of stool for the colonoscopy to be
performed. You will need to be on a low fiber diet a few days prior to the procedure,
and consume a special cleansing solution on the day before the examination. A
specific bowel cleansing instruction sheet will be given, and it is important to follow the instructions carefully in order for the colon to be completely clean for the procedure to be accurate and comprehensive. If you do not complete the
preparation, it may be unsafe to perform the colonoscopy and the procedure may
have to be rescheduled. If you are unable to take the preparation, please contact the
clinic.
You will also need to be fasted for at least 6 hours prior to the procedure.
Certain medications need to be adjusted or avoided before the examination, so it is
best to inform your surgeon of all your current medications as well as allergies. If
you also have any major diseases, such as heart or lung diseases, please discuss this as you might require special attention during the procedure. You will be sedated during the procedure, so please arrange to have someone drive you home after the procedure. You should not drive or operate machinery until the
next day.
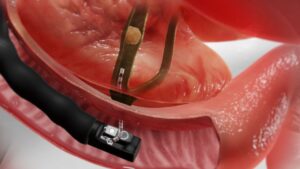
What can be expected during colonoscopy?
The procedure is usually well tolerated, but there is often a feeling of pressure,
gassiness, bloating or cramping at various times during the procedure. You will be given medication through a vein to help you relax and better tolerate any discomfort
that you may experience. You will be lying on your side or your back while the
colonoscope is advanced through the large intestine. The lining of the colon is
examined carefully while inserting and withdrawing the instrument. The procedure
usually lasts for 15 to 60 minutes. In rare instances, the entire colon cannot be
visualised and your surgeon could request for a supplementary test.
What if colonoscopy shows an abnormality?
If your surgeon sees an area that needs more detailed evaluation, a biopsy may be
obtained and submitted to a laboratory for analysis. Placing a special instrument
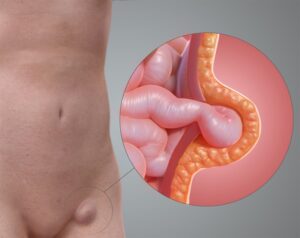
through the colonoscope to sample the lining of the colon does this. Polyps are
generally removed. The majority of polyps are benign (non-cancerous), but your
surgeon cannot always tell by the appearance alone. They can be removed by burning (fulgurating) or by a wire loop (snare). It may take your surgeon more than
one sitting to do this if there are numerous polyps or if they are very large. Sites of bleeding can be identified and controlled by injecting certain medications or
coagulating (burning) the bleeding vessels. Biopsies do not imply cancer, however,
removal of a colonic polyp is an important means of preventing colo-rectal cancer.
What happens after colonoscopy?
Your surgeon will explain the results to you after your procedure, but biopsy results
will typically take several days to return. You may have some mild cramping or
bloating from the air that was placed into the colon during the examination. This
should quickly improve with the passage of gas. You should be able to eat normally
the same day and resume your normal activities after leaving the hospital.
As you will be given sedatives during the procedure, you will be observed until most
of the effects have worn off (1-2 hours), and will need someone to drive you home
after. Do not drive or operate machinery until the next day, as the sedatives given
will impair your reflexes. If you do not remember what your surgeon told you about
the examination or follow-up instructions, call the clinic that day or the next to find
out what you were supposed to do. If polyps were found during the colonoscopy, you will need to have a repeat
procedure, and your surgeon will decide on the frequency of the examination.
What complications can occur?
Colonoscopy and biopsy are safe. While complications are uncommon, they can
occur. They include bleeding (1 in 1000) from the site of a biopsy or polypectomy
and a tear (perforation; 1 in 1500) through the lining of the bowel wall. Should this
occur, it may be necessary for your surgeon to perform abdominal surgery to repair
the tear. Blood transfusions are rarely required. A reaction to the sedatives can
occur. Irritation to the vein that medications were given is uncommon, but may
cause a painful lump lasting a few weeks. Warm, moist towels will help relieve this
discomfort.
It is important to contact the clinic if you notice symptoms of severe abdominal pain,
fevers, chills or rectal bleeding of more than one-half cup. Bleeding can occur up to
several days after a biopsy.
While colonoscopy is the best test for excluding colorectal cancer and polyps, there is
still a <3% that these may be missed by the procedure.
Are there any alternatives to colonoscopy?
There are also alternatives to colonoscopy, such as the CT colonography and the
double contrast barium enema. However, these alternative investigations might not
be as accurate in detecting small polyps, and also carry the potential risk of radiation exposure. Furthermore, you will be advised to have a colonoscopy should there be any abnormalities found on these alternative investigations. The risk of perforation, however, is much lower in comparison.