Is surgery the only treatment option for colon cancer?
There are various treatment options for colon cancer that are not limited to just
surgery.
However, these treatment options are mostly used as adjuncts to surgery, meaning
that they are used in addition to surgery, especially if a long-term solution is sought after.
These adjuncts include chemotherapy, targeted therapy, immunotherapy and
radiation therapy.
What forms of surgery for colon cancer are there?
In situations where the cancer is still at a very early stage, local excision can be
undertaken. This involves cutting the cancer using a colonoscopy, or through the
rectum without the need for any incision through the abdominal wall.
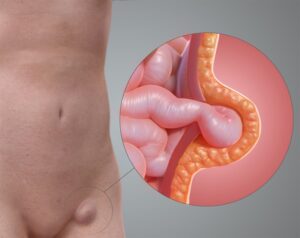
In other situations where the cancer is larger, a more extensive resection is
undertaken to remove the tumour. This resection is termed as a colectomy, with variations depending on how much and which part of the colon is removed. During a colectomy, the surrounding
lymph nodes are simultaneously removed. After the diseased segment is removed, the ends of the colon will be reconnected in a joint called the anastomosis. There are circumstances when a part of
an intestine needs to be put to empty outside the abdomen. This external opening is called a stoma and is
meant for waste to be passed out from the body.
How is colectomy surgery for colon cancer performed?
Most colon cancer operations are performed with keyholes, which is also known as laparoscopy. This involves the use of specially designed instruments that pass through much smaller cuts on the abdomen, without the need for a long cut as it was traditionally so.
Laparoscopic colectomy surgery allows faster recovery with less pain, compared to open (larger cut) surgery.
These surgeries are always performed under general anaesthesia, with operation
times depending on the complexity of the procedure.
What are the risks of colectomy surgery for colon cancer?
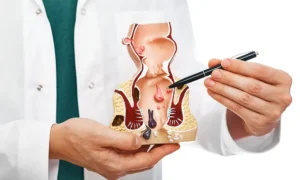
Other than for the risks of general anaesthesia, the main risks of colectomy surgery
centre around anastomotic leakage, bleeding and bowel obstruction.
Anastomotic leakage happens when the seal between 2 ends of the joined colon do not mend properly. This is a potentially catastrophic complication that requires
further surgical intervention to remedy.
Will I need a stoma after colon cancer surgery?
There are situations following colectomy that an anastomosis leak can be potentially
more devastating or likely. In these cases, there is a chance that a temporary stoma
is recommended to divert the flow of waste, to mitigate the potential risks.
There are also circumstances where the situation presents itself as impossible or too
risky for an anastomosis to be made. An example of the former is when the controlling mechanism of
bowel movement in the anus needs to be removed for complete cancer resection. An example of the
latter is during a complicated surgery where it is too
risky to prolong the duration of surgery.
The aim of colectomy surgery for colon cancer is to achieve the completeness of
cancer removal balanced with the quality of life. While having a stoma can potentially be a
set-back for some, a decent quality of life can be achieved with a positive mindset
and good nursing care.
What is recovery like after colectomy surgery for colon cancer?
Depending on the duration and complexity of operation, most patients are able to
commence a soft diet within 3-4 days of operation. There might be some drainage and intravenous tubes connecting that will be removed in the course of recovery.
Early mobilisation in terms of getting out of bed and walking, with deep breathing
exercises, are greatly encouraged.
Will I have difficulties controlling my bowels after colectomy surgery for colon cancer?
Most patients will not have any issue with controlling bowels after colectomy surgery.
However, some patients might experience more frequent bowel movements, depending on the length of colon removed.