What is Colorectal Surgery?
Colorectal surgery refers to surgical procedures performed on the colon (large intestine) and rectum. These surgeries are typically performed to treat a variety of conditions, ranging from benign disorders to serious diseases such as cancer. Colorectal surgery can be performed using open surgery or minimally invasive techniques like laparoscopy.
Conditions Treated by Colorectal Surgery
Colorectal surgery can address several conditions, including:
Colorectal Cancer
A type of cancer that begins in the colon or rectum, often requiring surgical removal of the tumour and surrounding tissue.
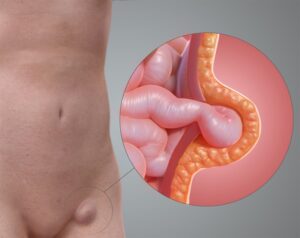
Diverticulitis
Inflammation or infection of small pouches (diverticula) that can form in the walls of the colon, sometimes necessitating surgery if complications arise.
Inflammatory Bowel Disease (IBD)
Chronic conditions like Crohn’s disease and ulcerative colitis cause inflammation of the digestive tract, which may require surgery to remove affected portions.
Polyps
Non-cancerous growths on the lining of the colon or rectum may be removed to prevent them from becoming cancerous.
Rectal Prolapse
A condition where the rectum slips outside the anus, often corrected with surgery.
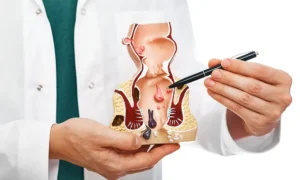
Haemorrhoids
Swollen veins in the lower rectum or anus that may require surgical treatment if severe.
Types of Colorectal Surgery
There are several types of colorectal surgeries, each tailored to treat specific conditions. Some of the common procedures include:
Colectomy
Surgical removal of all or part of the colon. A partial colectomy removes a segment of the colon, while a total colectomy removes the entire colon. This procedure is often used to treat colon cancer, severe IBD, or diverticulitis.
Proctectomy
The surgical removal of all or part of the rectum, commonly performed to treat rectal cancer.
Colostomy
Creating an opening (stoma) in the abdominal wall to divert waste from the colon to a colostomy bag. This may be temporary or permanent, depending on the underlying condition.
Polypectomy
The removal of polyps from the colon or rectum, often performed during a colonoscopy.
Hemorrhoidectomy
Surgical removal of severe haemorrhoids that have not responded to other treatments.
Strictureplasty
Surgical widening of narrowed sections of the intestines, commonly performed in patients with Crohn’s disease.
Preparing for Colorectal Surgery
Surgical widening of narrowed sections of the intestines, commonly performed in patients with Crohn’s disease.
Pre-Surgical Evaluations
Your doctor will conduct a thorough medical evaluation, including physical exams, blood tests, imaging studies (such as CT scans or MRIs), and possibly colonoscopy to assess your condition and determine the best surgical approach.
Medications
You may be instructed to stop certain medications before surgery, especially blood thinners, to reduce the risk of bleeding. Your doctor will provide specific guidelines.
Bowel Preparation
Before surgery, you may need to follow a special diet and take laxatives to empty your bowels. This is crucial for reducing the risk of infection and making the surgery easier to perform.
Fasting
You will need to fast for a specified period before surgery, usually starting the night before, to ensure your stomach is empty.
What to Expect During Surgery
Colorectal surgeries can be performed using traditional open surgery or minimally invasive techniques such as laparoscopy. The choice depends on the specific condition, the patient’s health, and the surgeon’s expertise.
Anaesthesia
You will receive general anaesthesia, ensuring you are asleep and pain-free throughout the procedure.
Surgical Procedure
The duration and complexity of the surgery will vary based on the type of surgery being performed. Minimally invasive surgeries generally have shorter recovery times and less postoperative pain compared to open surgeries.
Monitoring
Throughout the surgery, your vital signs will be closely monitored to ensure your safety.
Recovery After Colorectal Surgery
Recovery times and post-surgical care will vary based on the type of surgery and individual factors. Here’s what to expect:
- You may need to stay in the hospital for a few days to a week, depending on the surgery and your recovery progress. During this time, your medical team will monitor your vital signs, manage pain, and watch for any complications.
- Initially, you will be on a liquid diet, gradually transitioning to soft foods as your digestive system heals. Your doctor or a dietitian will provide specific dietary guidelines to follow.
- Light activity and walking are encouraged to promote circulation and prevent blood clots. However, you should avoid strenuous activities and heavy lifting for several weeks.
- Regular follow-up appointments are essential to monitor your recovery, address any concerns, and adjust medications if needed.
Caring for Yourself at Home
Proper care at home is crucial for a smooth recovery:
- Keep surgical wounds clean and dry. Follow your doctor’s instructions on how to care for your incisions and watch for signs of infection, such as redness, swelling, or discharge.
- Take prescribed pain medications as directed. Over-the-counter pain relievers may also be recommended for managing mild discomfort.
- Follow your doctor’s dietary recommendations. Eating small, frequent meals can help ease digestion and prevent discomfort.
- Stay well-hydrated by drinking plenty of fluids, unless otherwise advised by your doctor.
- Ensure you get plenty of rest to help your body heal. Listen to your body and avoid overexertion.
Potential Complications
While colorectal surgery can be highly effective, it does carry risks, as with any major surgery. Potential complications include:
Infection
Surgical site infections or internal infections can occur, requiring antibiotics or additional treatment.
Potential Complications
While colorectal surgery can be highly effective, it does carry risks, as with any major surgery. Potential complications include:
Bleeding
Excessive bleeding during or after surgery may necessitate blood transfusions or further surgery.
Bowel Obstruction
Scar tissue from surgery can sometimes cause bowel obstructions, requiring further treatment.
Anastomotic Leak
A leak at the site where the intestines are reconnected can occur, potentially requiring additional surgery to repair.
Blood Clots
Deep vein thrombosis (DVT) or pulmonary embolism (PE) can develop, necessitating measures to prevent clots, such as blood thinners and compression stockings.