What is Gastrointestinal Bleeding?
Gastrointestinal bleeding occurs anywhere in the gastrointestinal tract, including the oesophagus, stomach, small intestine, and large intestine (colon). It can range from mild to severe and may present as visible blood in stool or vomit or as invisible blood detected through laboratory testing.
Common Causes of Gastrointestinal Bleeding
There are several potential causes of gastrointestinal bleeding, including:
- Peptic Ulcers – Open sores in the stomach lining or small intestine.
- Gastritis – Inflammation of the stomach lining, often caused by infection or irritation.
- Oesophageal – Enlarged veins in the oesophagus, often due to liver disease.
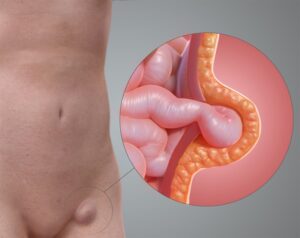
- Diverticulosis – Small pouches that develop in the colon and may bleed if inflamed or infected.
- Colon Polyps or Cancer – Abnormal growths in the colon or rectum that can bleed.
- Haemorrhoids (Piles) – Swollen blood vessels in the rectum or anus.
Symptoms of Gastrointestinal Bleeding
The symptoms of gastrointestinal bleeding can vary depending on the location and severity of the bleeding, but may include:
- Visible Blood – Bright red blood in the stool or black, tarry stools (melena).
- Vomiting Blood – Blood in vomit, which may appear red or have a coffee-ground-like appearance.
- Fatigue – Feeling tired or weak due to blood loss.
- Abdominal Pain – Discomfort or cramping in the abdomen.
When to Seek Medical Attention
Gastrointestinal bleeding can be a medical emergency, especially if it is severe or persistent. Seek immediate medical attention if you experience:
- Profuse or uncontrollable bleeding from the rectum or vomit.
- Symptoms such as dizziness, lightheadedness, rapid heartbeat, or pale, clammy skin.
- Severe abdominal pain, especially if it is accompanied by bleeding.
Diagnosing Gastrointestinal Bleeding
To diagnose gastrointestinal bleeding, your doctor will perform a thorough evaluation, which may include:
- Your doctor will ask about your symptoms, medical history, and any recent changes in diet or lifestyle.
- Your abdomen will be examined for tenderness, swelling, or signs of bleeding.
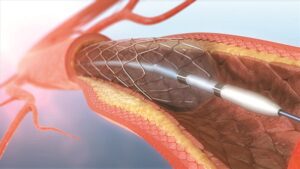
- Additional tests may be ordered, such as blood tests, stool tests, upper endoscopy, colonoscopy, or imaging studies (CT scan, angiography) to identify the source and severity of the bleeding.
Treatment Options for Gastrointestinal Bleeding
Treatment for gastrointestinal bleeding depends on the underlying cause and severity. Options may include:
Medications
This treatment option involves using proton pump inhibitors (PPIs), antacids, or antibiotics. PPIs work by reducing the production of stomach acid, helping to heal peptic ulcers and prevent further bleeding. Antacids neutralise stomach acid and relieve symptoms, while antibiotics may be prescribed to treat bacterial infections contributing to gastrointestinal bleeding.
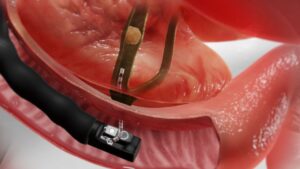
Endoscopic Therapy
Endoscopic therapy is a minimally invasive procedure that uses an endoscope, a flexible tube with a camera, and specialised tools. During endoscopic therapy, a gastroenterologist can directly visualise the source of bleeding and perform interventions to stop it. This may include techniques such as endoscopic cauterisation, where heat or electrical current is used to seal off bleeding blood vessels, or banding, where small rubber bands are placed around varices or other sources of bleeding to constrict and stop the bleeding.
Surgery
In cases of severe or persistent bleeding that cannot be controlled with medication or endoscopic therapy, surgical intervention may be necessary. Surgical options for gastrointestinal bleeding may include procedures to repair or remove the affected tissue. For example, in cases of peptic ulcers or diverticular bleeding, surgery may involve removing the affected portion of the stomach or intestine. In severe cases of gastrointestinal bleeding, such as massive haemorrhage or trauma, emergency surgery may be required to stop the bleeding and stabilise the patient.
Recovery and Prognosis
The prognosis for gastrointestinal bleeding depends on factors such as the cause, severity, and promptness of treatment. Most people recover well with appropriate treatment and monitoring. After treatment, it’s essential to follow any dietary or lifestyle recommendations provided by your doctor to prevent recurrence and promote healing.
Gastrointestinal bleeding can be a concerning symptom that requires prompt medical attention. If you experience symptoms such as blood in the stool or vomit, abdominal pain, or signs of shock, seek immediate medical care. Early diagnosis and treatment offer the best chance for successful outcomes and reduce the risk of complications. Remember, your health is important, and proactive management of gastrointestinal bleeding can help ensure the best possible outcomes and a speedy recovery.
If you have any concerns or questions about gastrointestinal bleeding or digestive health, don’t hesitate to reach out to your doctor or healthcare provider. Your proactive involvement in your healthcare journey can make a significant difference in your overall well-being.